Device Recommendation for Sleep Apnea & Snoring
Answer the questions below:
Obstructive sleep apnea (OSA) is a condition that affects millions of people worldwide, causing disrupted sleep, daytime sleepiness, and other health issues. With its increasing prevalence, it’s crucial to find an effective treatment that suits each individual’s needs.
Tongue-stabilizing devices (TSDs) and mandibular advancement devices (MADs) are two options that have gained attention in recent years. But which one is the better solution for OSA? Let’s put them head-to-head in a “TSD vs MAD” comparison and find out.
Key Takeaways
-
TSD and MAD therapies are both effective treatment options for Obstructive Sleep Apnea, with MAD therapy having better results in terms of reducing daytime sleepiness and improving quality of life.
-
Patient acceptance and adherence should be considered when selecting a treatment option due to potential side effects such as discomfort, excessive salivation, dry mouth or pain/discomfort in teeth.
-
Alternative treatments include CPAP therapy, positional therapy & lifestyle modifications. Consulting a doctor is recommended for best results.
Understanding TSD and MAD
TSDs and MADs are innovative devices designed to alleviate snoring and sleep apnea by enlarging the airway, thus improving sleep quality and reducing daytime sleepiness.
In a randomized controlled trial conducted at a tertiary hospital sleep clinic, as a part of clinical research in respiratory medicine, a comparative analysis was conducted between the two treatment arms: TSD and MAD, utilizing home sleep apnea testing and patient-reported outcomes to evaluate their effectiveness.
Tongue-Stabilizing Devices (TSDs)
The novel tongue stabilizing device, or tongue-retaining device, is a non-invasive treatment option for OSA. The mechanism of action for TSDs involves a small compartment that suctions the tongue in place, preventing it from falling back into the throat and obstructing the airway. The TSD used in the clinical trial was Aveo-TSD, which underwent a titration protocol to adjust the degree of tongue protrusion and ensure the best possible treatment outcome.
The trial revealed that TSD therapy had a positive response to the respiratory event index, oxygen desaturation index, and fatigue measures. However, the acceptance rate of TSD therapy was low, with only 50% of patients being able to tolerate the treatment.
Mandibular Advancement Devices (MADs)
Mandibular advancement devices, also known as mandibular advancement device mad, are another type of oral appliance used to treat OSA. They work by physically shifting the jaw forward, increasing the size of the airway and enabling better airflow. One such device is the mandibular advancement splint. MADs often require a prescription and are custom-made to fit the patient’s mouth. Oral appliance therapy, specifically using mandibular advancement devices, has proven to be an effective treatment option for many patients.
MAD therapy has been shown to result in significant improvements in daytime sleepiness and quality of life measures. The MAD therapy lasted averaged 88 days after insertion. There was a variance of 54 days. However, potential drawbacks include potential jaw pain and stiffness, drooling, and other adverse effects.
Efficacy of TSD vs MAD
When comparing the effectiveness of TSD and MAD therapies in treating OSA, the results of the clinical trial showed that both treatments had a comparable efficacy in terms of respiratory event index and fatigue reduction. However, MAD therapy achieved better results in terms of reducing daytime sleepiness and improving quality of life.
A complete or partial response to TSD therapy was observed in 62.9% of patients. On the other hand, MAD therapy demonstrated significant improvement in daytime sleepiness, as measured by the Epworth Sleepiness Scale (ESS), and better results in the Functional Outcomes of Sleep Questionnaire (FOSQ-10) total score. In fact, patients reported improvements in both ESS and FOSQ-10 scores.
Despite the comparable efficacy of TSD and MAD therapies in certain aspects, the acceptance rate of TSD therapy was found to be low. There is a good chance that the low acceptance rate for TSD treatment after two months was significantly impacted by discomfort and negative outcomes. These factors likely contributed to many people dropping out of the treatment.
Patient Acceptance and Adherence
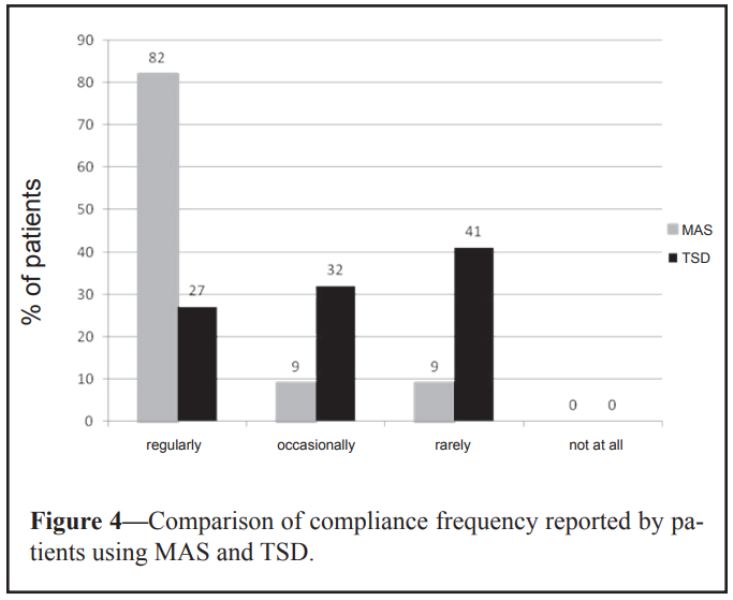
Patient acceptance and adherence are important factors to consider when comparing TSD and MAD therapies. The clinical trial found that patients achieved different results with these therapies:
-
TSD users had a lower acceptance rate and self-reported adherence when compared to MAD users
-
TSD users experienced adverse effects more often than MAD users
-
This was reported by the users themselves
The low acceptance rate of TSD therapy was, in part, due to the discomfort experienced by the patients. This discomfort had a damaging effect on the rate of acceptance.
Commonly reported adverse effects among TSD users included discomfort due to the device not remaining in place, excessive salivation, and a strong sensation on the tongue. MAD users voiced dryness of mouth and teeth discomfort or pain as the most common adverse effects. This is in contrast to other reports..
Evaluating patient preferences and the potential for discomfort is key when selecting an OSA treatment option. The trial results suggest that the choice between TSD and MAD therapies may depend on individual tolerance and the ability to cope with potential side effects.
Side Effects and Risks
Both TSD and MAD therapies come with potential side effects and risks that patients should be aware of before choosing a treatment option. For TSD therapy, the most commonly reported adverse effects were discomfort due to the device not remaining in place, excessive salivation, and a strong sensation on the tongue. Users of MAD often reported dry mouth and pain or discomfort in teeth as the main unpleasant side effects. However, these patients still tend to use it as the preferred solution..
In addition to the discomfort and oral symptoms, TSD therapy was associated with an average rise in systolic/diastolic blood pressure, while MAD therapy led to an average decrease in blood pressure. Considering the potential risks and side effects of each treatment option and discussing them with your healthcare provider before deciding is significant.
Cost and Accessibility
The costs and accessibility of TSD and MAD therapies may also be a determining factor for patients seeking OSA treatment. Over-the-counter TSDs and MADs generally fall between $50 and $150, while custom-made MADs can range from $1,800 to $3,000, including the appliance, dental visits, and post-treatment follow-ups.
While costs can vary, remember that health insurance may cover the expense of TSD or MAD devices. However, coverage is not guaranteed, and it is advisable to contact your insurance provider to determine what coverage is available.
Cleaning and Longevity
Maintaining and caring for your TSD or MAD device is key to ensuring its effectiveness and longevity. The recommended cleaning procedure for both devices involves sterilizing them with hot water after each use and cleaning them regularly to avoid the accumulation of harmful bacteria.
The average lifespan of a TSD is approximately 106 days before needing to be replaced, while a MAD generally requires replacement after approximately 3 years of use. Proper care and maintenance can help prolong the lifespan of your device and ensure optimal treatment results.
Choosing the Right Treatment Option
When selecting the most appropriate treatment option for OSA, considering factors such as:
-
the severity of the condition
-
patient preference
-
effectiveness of the treatment
-
potential side effects
-
lifestyle factors
-
cost and accessibility
is vital. Consulting with your doctor before acquiring a TSD or MAD device is important, as they can help determine the most suitable treatment for your individual needs.
The severity of OSA is a key factor in determining the most appropriate treatment. For mild cases, a broader range of treatment options is available, while for moderate to severe cases, continuous positive airway pressure (CPAP) therapy is usually the preferred choice. However, alternative treatments, such as TSD and MAD therapies, can also be considered depending on the patient’s preferences and individual circumstances.
Alternative Treatments for Obstructive Sleep Apnea
Aside from TSD and MAD therapies, there are other treatment options available for sleep disordered breathing, such as OSA. Continuous positive airway pressure (CPAP) therapy is the most commonly prescribed treatment for moderate to severe OSA, which is one of the sleep related breathing disorders. It involves wearing a mask over the nose and/or mouth, which delivers a constant stream of air to keep the airway open during sleep.
Positional therapy can also be effective for some OSA patients, particularly those who experience worsened symptoms when sleeping in certain positions. This therapy involves using specialized pillows or devices to maintain a specific sleep position that reduces airway obstruction.
Lifestyle modifications that may help reduce OSA symptoms include:
-
Weight loss
-
Abstaining from smoking
-
Reducing alcohol intake
-
Sleeping on one’s side to improve sleep breath
Discussing all available treatment options, including innovative health technologies, with your healthcare provider to determine the best course of action for your specific needs is crucial.
Summary
In conclusion, both TSD and MAD therapies offer potential benefits for individuals suffering from OSA. While TSD therapy has shown promising results in reducing respiratory events and fatigue, MAD therapy demonstrated superior outcomes in reducing daytime sleepiness and improving quality of life.
Ultimately, the choice between TSD and MAD therapies depends on individual factors, including patient preference, tolerance of potential side effects, and financial considerations.
By carefully evaluating all available options, patients can make an informed decision and find the most effective treatment for their OSA.
Frequently Asked Questions
What is the difference between mad and TSD snoring?
MAD and TSD snoring mouthpieces both offer solutions to stop snoring, but they work differently. The MAD is worn like a denture and advances the lower jaw forward to widen the airway, while the TSD gently pulls out the tongue to open up the pathway.
What is the difference between mad and TRD?
MADs move the jaw forward while TRDs hold the tongue in place, making them two distinct anti-snoring solutions. Whether you should opt for one of these devices is something you can determine after researching both.
How effective is mad for sleep apnea?
MADs have been proven to be an effective solution for sleep apnea, with effectiveness being about 65-80% that of a CPAP device. In studies comparing user-compliance rates between the two, MADs come out on top every time.
Can health insurance cover the cost of TSD and MAD devices?
Health insurance may cover the cost of TSD or MAD devices, but it is best to contact your provider to determine what coverage is available.
How often should TSD and MAD devices be replaced?
TSDs should be replaced every 106 days, while MADs should be replaced after 3 years of use.
References
- Comparison of Mandibular Advancement Splint and Tongue Stabilizing Device in Obstructive Sleep Apnea: A Randomized Controlled Trial. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2675900/
- Comparative Effects of Two Oral Appliances on Upper Airway Structure in Obstructive Sleep Apnea. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3065257/
- The Tongue-Retaining Device: Efficacy and Side Effects in Obstructive Sleep Apnea Syndrome. https://jcsm.aasm.org/doi/full/10.5664/jcsm.27598


