Have you ever wondered how a good night’s sleep can affect your life? Or how a lack thereof can lead to major health problems, including memory loss and cognitive decline? The answer lies in a common but often overlooked sleep disorder known as sleep apnea and memory issues are often associated with it.
Key Takeaways
-
Sleep apnea, particularly central sleep apnea, leads to cognitive decline and memory loss due to oxygen deprivation and disrupted REM sleep, which can be mitigated with appropriate treatments like CPAP therapy.
-
Obstructive Sleep Apnea (OSA) is a common sleep disorder characterized by blocked upper airway, leading to breathing disruptions with signs including excessive daytime sleepiness and loud snoring, and is linked to serious health issues such as cardiovascular disease and diabetes.
-
Effective management of sleep apnea with treatments like CPAP therapy, oral appliances, lifestyle changes, or possibly surgery can improve memory function, cognitive performance, and overall health, reducing risks of high blood pressure, type 2 diabetes, and Alzheimer’s disease.
The Impact of Sleep Apnea on Cognitive Functions

Sleep apnea, especially central sleep apnea, significantly affects cognitive functions including memory, attention, and executive functioning. It’s not just about feeling groggy or unrefreshed in the morning. The effects of this sleep disorder reach far beyond fatigue, leading to cognitive decline and memory loss, especially when it remains untreated.
But there’s a silver lining. Appropriate treatment, such as continuous positive airway pressure (CPAP) therapy, may help restore memory function to a degree.
The Role of Oxygen Deprivation
So, how does sleep apnea lead to cognitive decline? One of the key contributors is oxygen deprivation. When you have sleep apnea, your breathing repeatedly stops and starts during sleep, leading to periods of oxygen deprivation. This lack of oxygen to the brain is the primary cause of brain injury and memory loss associated with sleep apnea.
The effects of this oxygen deprivation aren’t just immediate; they have long-term consequences. Short-term effects include memory difficulties and impaired concentration. Long-term effects can lead to a reduced attention span, fatigue, daytime drowsiness, and challenges in cognitive functions such as reasoning and emotion regulation.
Encouragingly, brain damage and memory loss can be reversed with effective treatment for sleep apnea.
Disrupted REM Sleep and Its Consequences
Disruption of REM sleep is another significant factor causing memory loss in sleep apnea patients. REM sleep is an essential part of our sleep cycle, playing a crucial role in memory consolidation. It helps to strengthen our declarative memory and allows memory traces to disengage from the hippocampus over time.
Sleep apnea, however, disrupts this process, impacting the hippocampus’s signaling pathways, which are necessary for memory consolidation. The long-term consequences of this disruption can be severe, leading to diminished academic performance, behavioral issues, and a decrease in overall quality of life, particularly in adolescents and children.
Daytime Drowsiness and Cognitive Performance
As if the memory issues and cognitive decline weren’t enough, sleep apnea also leads to severe daytime drowsiness and fatigue. This is a direct result of the lack of restorative sleep at night, owing to the frequent pauses in breathing.
Daytime drowsiness significantly impairs cognitive performance, leading to memory problems. This, in turn, affects daily functioning, mood, and quality of life, and can even result in reduced work productivity.
Understanding Sleep Disorders: Focus on Obstructive Sleep Apnea (OSA)
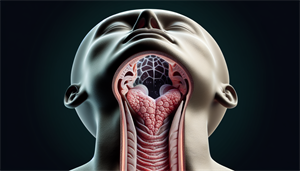
Now that we’ve understood the impact of sleep apnea on memory and cognitive functions, let’s focus on a specific type of sleep apnea, known as Obstructive Sleep Apnea (OSA). OSA is a prevalent sleep disorder that occurs when the upper airway becomes blocked, leading to breathing disruptions during sleep.
Identifying and treating OSA is important given its association with various serious health concerns including cardiovascular disease, diabetes, and glaucoma. Furthermore, it can increase the risk of premature mortality.
How the Upper Airway Becomes Blocked
The blockage of the upper airway in OSA is attributed to:
-
Altered upper airway structure and muscular function
-
A low arousal threshold
-
Increased fat deposits around the upper airway
-
Changes in breathing patterns
Specifically, the muscles in the back of the throat are important. In OSA, these muscles relax excessively, leading to breathing difficulties. This leads to serious consequences such as loud snoring, caused by air squeezing through a narrowed or blocked airway, and interrupted breathing, or apneas, which occur when the airway is completely or partially blocked, cutting off the air supply.
Recognizing the Signs of Severe Sleep Apnea
Identifying the signs of severe sleep apnea is imperative for effective management of the disorder. The primary indicators include:
-
Excessive daytime sleepiness
-
Loud snoring
-
Observed episodes of stopped breathing during sleep
-
Waking during the night
-
Frequently waking up to urinate at night
-
Morning headaches
-
Dry mouth or sore throat
Gasping for air during sleep is a direct consequence of the breathing interruptions caused by obstructive sleep apnea, where the airway collapses or becomes obstructed, requiring a forceful effort to resume breathing. The excessive daytime sleepiness in individuals with severe sleep apnea is primarily attributed to the disrupted and poor quality sleep resulting from sleep breathing problems, such as frequent pauses in breathing during the night.
Treatments That Can Help Keep the Airway Open
Thankfully, multiple treatments exist that can effectively manage sleep apnea by ensuring the airway remains open. The most common and effective treatment is Continuous Positive Airway Pressure (CPAP) therapy, which involves using a machine to provide a continuous flow of air, preventing the airway from collapsing during sleep.
Alternative treatments include oral appliances, which work by repositioning the jaw and tongue to remove physical blockages from the upper airway, and lifestyle changes such as weight loss and increased physical activity.
CPAP Therapy: The Frontline Treatment
CPAP therapy is a vital tool in the treatment of sleep apnea. It involves the use of:
-
a mask or nasal device during sleep
-
to deliver a continuous flow of air
-
thereby maintaining an open airway
-
and preventing the breathing disturbances associated with obstructive sleep apnea.
While CPAP therapy is quite effective, it should be noted that some individuals may have trouble adhering to it due to discomfort caused by wearing the mask or nasal device.
Alternatives to CPAP: Oral Appliances and Lifestyle Changes
While CPAP is the primary treatment, alternatives exist for those who find it uncomfortable or challenging to use. Oral appliances, for example, work by repositioning the jaw and tongue to remove physical blockages from the upper airway.
Another key aspect of managing sleep apnea involves lifestyle modifications. These include:
-
Weight loss
-
Increased physical activity
-
Abstaining from alcohol and tobacco
-
Avoiding certain medications
-
Adjusting sleep patterns to enhance sleep quality
When Surgery Might Be Necessary
In some cases, when other treatments are not effective or not well-tolerated, surgery might be necessary. Various types of sleep apnea surgeries are available, including:
-
Nasal surgery
-
Palate surgery
-
Tongue surgery
-
Nerve stimulation
-
Skeletal surgery
While surgery may not guarantee a complete cure, it has a success rate of 60 percent or higher, providing substantial advantages for patients. However, like any surgical procedure, it carries potential risks such as excessive bleeding, infection, and additional breathing problems.
The Relationship Between Sleep Apnea, Brain Health, and Alzheimer's Disease

Sleep apnea is not just a sleep disorder. Its implications extend beyond sleep quality and cognitive function to brain health and Alzheimer’s disease. Untreated sleep apnea can elevate the risk of developing Alzheimer’s, a progressive brain disorder that affects memory, thinking, and behavior.
Sleep apnea can potentially result in brain damage and the buildup of amyloid plaques due to intermittent drops in oxygen levels and disrupted sleep patterns, thus contributing to the onset of Alzheimer’s Disease.
Sleep Apnea as a Risk Factor for Alzheimer's
One significant factor connecting sleep apnea to Alzheimer’s disease is the accumulation of amyloid plaques in the brain. These pathological formations are closely related to Alzheimer’s disease, and have been identified in individuals with sleep apnea.
Yet, there is hope. Studies suggest that treating sleep apnea, particularly with positive airway pressure therapy, may potentially reduce the risk of Alzheimer’s Disease.
Protecting a Healthy Brain Through Early Intervention
The early treatment of sleep apnea has the potential to slow cognitive decline in individuals with untreated obstructive sleep apnea and comorbid conditions like Mild Cognitive Impairment (MCI) or Alzheimer’s Disease.
Early intervention, particularly through positive airway pressure (PAP) therapy, has the potential to reverse the white matter damage associated with severe sleep apnea. Moreover, consistent sleep apnea treatment has the potential to enhance memory function.
Real Stories: How Individuals Reclaimed Memory Function Post-Treatment

Real-world experiences provide proof of the beneficial effects of sleep apnea treatment. Many individuals have experienced significant improvement in memory and cognitive performance after receiving treatment for sleep apnea.
These improvements are not just anecdotal. Research indicates that consistent sleep apnea treatment results in improved memory function and rectified sleep EEG abnormalities, contributing to an overall improvement in daily life quality.
Addressing High Blood Pressure and Other Serious Health Issues Linked to Sleep Apnea
Treating sleep apnea doesn’t just improve sleep and cognitive function; it also brings significant benefits to overall health. For instance, individuals with sleep apnea have a higher likelihood of developing high blood pressure, which can further worsen sleep apnea.
Also, sleep apnea interferes with glucose metabolism and promotes insulin resistance, thereby affecting the development of type 2 diabetes due to the negative effects of oxygen deprivation on glucose levels.
Proactive Measures: Enhancing Daily Life with Better Sleep
Boosting sleep quality involves more than just treating sleep apnea. Taking proactive steps, such as setting a regular sleep routine and creating a comfortable sleep environment, can improve daily life and overall well-being.
In addition, lifestyle changes such as increasing physical activity, abstaining from alcohol and tobacco, avoiding certain medications, and adjusting sleep positions can enhance sleep quality.
Summary
Sleep apnea is more than a sleep disorder. It’s a significant health issue that affects cognitive function, memory, and overall brain health. Its links to Alzheimer’s disease underline the importance of early diagnosis and effective treatment. From CPAP therapy to lifestyle adjustments, there are numerous ways to manage sleep apnea, improve sleep quality, and protect brain health. Remember, a good night’s sleep is not just about feeling rested; it’s about safeguarding your cognitive abilities and living a healthier life.
Frequently Asked Questions
Does sleep apnea affect your memory?
Yes, sleep apnea can affect your memory and may be associated with a decline in cognitive impairment and memory loss, according to new studies. This was indicated by a study where individuals with sleep apnea were diagnosed with mild cognitive impairment almost ten years earlier than those without sleep breathing conditions.
Can sleep apnea cause personality changes?
Yes, sleep apnea can cause personality changes over time due to its impact on mental health and social interactions. It is essentially a condition that obstructs the airway during sleep.
Does CPAP add years to life?
Yes, studies show that CPAP therapy can reduce the risk of cardiovascular events and improve life expectancy after six or seven years of therapy. It was also found to be tied to a 62% decline in the odds for death over 11 years of follow-up.
Is sleep apnea a risk factor for Alzheimer's disease?
Untreated sleep apnea can increase the risk of developing Alzheimer's disease. It's important to seek treatment for sleep apnea (date not included).
Can the memory loss caused by sleep apnea be reversed?
Yes, memory loss caused by sleep apnea can be reversed to some extent with the right treatment, such as continuous positive airway pressure (CPAP) therapy. It's important to seek appropriate treatment as soon as possible.


