Have you ever experienced an irregular heartbeat during your sleep? This could be a symptom of sleep apnea heart palpitations, a disorder characterized by interrupted breathing during sleep, which can lead to heart palpitations. In essence, these are feelings of a racing or irregular heartbeat and can be quite disconcerting.
This blog post will guide you through understanding the link between sleep apnea and heart palpitations, their symptoms, risk factors, diagnosis, treatment, prevention, and much more!
Key Takeaways
-
Sleep apnea is a disorder characterized by repeated stopping and starting of breathing during sleep, which significantly impacts heart health, causing conditions such as myocardial ischemia, heart palpitations, and even heart attacks.
-
Risk factors for developing sleep apnea and heart palpitations include obesity, smoking, stress, hypertension, and diabetes, all of which can contribute to or exacerbate the severity of symptoms.
-
Treatment options to manage sleep apnea and heart palpitations range from Continuous Positive Airway Pressure (CPAP) therapy and lifestyle changes, such as weight loss and smoking cessation, to medications like beta blockers and anti-arrhythmic drugs.
Sleep Apnea and Heart Palpitations: The Connection

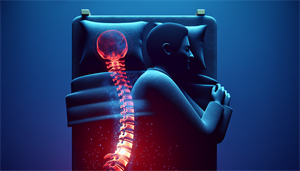
Sleep apnea is a medical disorder where breathing repeatedly stops and starts during sleep. This can have various detrimental effects on your heart, causing an irregular heartbeat, heart failure, and even heart attacks. Changes in blood oxygen levels during these episodes lead to a drop in heart rate during sleep and a subsequent increase upon waking to restore normal breathing. This ultimately leads to a medical condition known as myocardial ischemia, caused by insufficient oxygen supply.
Often, people with obstructive sleep apnea have nighttime heart palpitations. Some individuals may experience a stronger heartbeat, while others may notice variations in their heart rate and rhythm. These sensations are common and can be caused by a variety of factors. These palpitations result from changes in intrathoracic pressure and blood oxygen levels, which activate the sympathetic and parasympathetic systems. Sleep apnea, being a type of sleep disordered breathing, can lead to these fluctuations and changes.
Obstructive Sleep Apnea
Obstructive Sleep Apnoea (OSA), also known as obstructive sleep apnea, is the most common type of sleep apnea. It is characterized by:
-
Brief pauses in breathing during sleep
-
Blocked airway when the muscles supporting the soft tissues in the throat collapse
-
Obstruction in the airway primarily caused by complete or partial collapse of the airway
-
Often linked to anatomical abnormalities or the temporary relaxation of throat muscles
Symptoms of Obstructive Sleep Apnea include:
-
Daytime fatigue
-
Loud snoring
-
Disruptive sleep with snorting or gasping episodes
-
Gastroesophageal reflux disease (GERD), which can exacerbate the symptoms and increase the risk of heart palpitations; acid reflux is a common symptom of GERD
-
Weight gain, which plays a role in the development of sleep apnea, with fat accumulation in the neck area potentially obstructing breathing.
Central Sleep Apnea
Conversely, Central Sleep Apnea (CSA) is a severe condition marked by disrupted breathing during sleep. This is caused by the brain’s failure to send signals to the breathing muscles, causing individuals to stop breathing for brief periods during sleep. This lack of communication between the brain and the muscles responsible for breathing can lead to inadequate ventilation, compromised gas exchange, and an increased likelihood of experiencing heart palpitations.
CSA is often linked to severe illnesses, particularly those impacting the lower brainstem, which is responsible for regulating breathing. It has been found to be independently linked to nocturnal cardiac arrhythmias, and a higher severity of Central Sleep Apnea is correlated with an increased likelihood of experiencing heart palpitations.
Symptoms of Sleep Apnea-Induced Heart Palpitations

Sleep apnea-induced heart palpitations can manifest in various ways. During the night, you might experience slow heart rhythms (bradyarrhythmias) and unusually fast beating or fluttering of the heart. These symptoms can cause discomfort and disrupt your sleep, leading to further complications if not addressed promptly.
During the day, these symptoms might persist. Individuals with sleep apnea-induced heart palpitations may still encounter:
-
Slow heart rhythms
-
Sensations of heart fluttering
-
Sensations of heart racing
-
Sensations of heart pounding
-
Sensations of heart skipping beats
These symptoms can affect your daily activities and overall quality of life, emphasizing the importance of early diagnosis and treatment.
Nighttime Symptoms
Nighttime symptoms of heart palpitations induced by sleep apnea include slow heart rhythms (bradyarrhythmias) and unusually fast beating or fluttering of the heart. Hypoxia-induced inflammatory remodeling of adipose tissue, intermittent hypoxia, hypercapnia, intrathoracic pressure shifts, hyperactivity of the autonomic nervous system, and abrupt surges in heart rate are the mechanisms through which sleep apnea induces irregular heartbeat during the night.
Sleep apnea can also cause chest pain during the night. Shortness of breath during sleep in individuals with sleep apnea-induced heart palpitations may stem from intermittent breathing pauses, leading to reduced oxygen levels and cardiac strain. It’s essential to differentiate these symptoms from those of other conditions.
The nighttime symptoms of sleep apnea-induced heart palpitations may manifest as sensations of:
-
fluttering
-
racing
-
pounding
-
skipping beats
These sensations are associated with the onset of abnormal heart rhythms.
Daytime Symptoms
Daytime symptoms of sleep apnea-induced heart palpitations include fatigue, dizziness, and difficulty concentrating. Sleep apnea can result in daytime fatigue and sleepiness due to disruptions in breathing during sleep, leading to frequent awakenings that hinder restful sleep.
Difficulty concentrating during the day may be due to the frequent fluctuations in oxygen levels caused by sleep apnea, leading to significant stress on the body, known as oxidative stress, as well as the association between sleep apnea and heart rate fluctuations. Dizziness can also occur due to sleep apnea leading to cardiac arrhythmia and conduction disturbances. Typical daytime symptoms include slow heart rhythms (bradyarrhythmias), fluttering in the chest, or unexplained pounding heart sensations.
Risk Factors for Developing Sleep Apnea and Heart Palpitations
Understanding the risk factors for sleep apnea and heart palpitations aids in making better health decisions. Lifestyle factors such as excessive weight, stress, and specific medications can potentially contribute to the development of sleep apnea and heart palpitations.
Obesity is a significant risk factor, leading to:
-
Insulin resistance
-
Hyperleptinemia
-
Endothelial dysfunction
-
Systemic inflammation
All of these can increase the risk of sleep apnea and heart palpitations.
Smoking can also increase the susceptibility to heart palpitations, including atrial fibrillation, which can be intensified by the habit of smoking.
Additionally, untreated sleep apnea puts individuals at a heightened likelihood of developing hypertension, which can impose substantial strain on the cardiovascular system and result in complications such as heart palpitations.
Lifestyle Factors
Lifestyle choices significantly influence the risk of developing sleep apnea and heart palpitations. Obesity significantly contributes to the causal relationship between sleep apnea and cardiovascular disease. Both sleep apnea and obesity independently elevate the risk of health conditions that have adverse effects on heart health.
Smoking exacerbates the risk of cardiovascular disease by causing oxidative stress and endothelial dysfunction, and is linked to a heightened risk of atrial fibrillation or irregular, rapid heartbeat. These effects further elevate the existing risks in individuals with obstructive sleep apnea, resulting in increased cardiovascular morbidity. Alcohol consumption can also exacerbate the risk of sleep apnea and heart palpitations, and also elevate the probability of atrial fibrillation.
Unhealthy lifestyle factors that are linked to an elevated risk of developing sleep apnea, heart palpitations, and other cardiovascular conditions include:
-
High blood pressure
-
Poor cholesterol levels
-
Diabetes
-
Obesity
-
Symptoms of insomnia
-
Daytime sleepiness
-
Poor diet
Physical inactivity is also a significant contributing factor to the likelihood of experiencing sleep apnea and heart palpitations.
Medical Conditions
Certain medical conditions can also elevate your risk of sleep apnea and heart palpitations. Hypertension is a significant risk factor, with individuals with sleep apnea frequently having underlying hypertension. Many individuals with hypertension, particularly resistant hypertension, may also experience sleep apnea.
Diabetes significantly increases both the risk and severity of sleep apnea, subsequently elevating the likelihood of experiencing cardiac arrhythmias, a common cause of heart palpitations. Metabolic syndrome and obstructive sleep apnea (OSA) have a tendency to coexist, intensifying the impact of each other. Disruptions linked to OSA, such as elevated resting heart rates, indicate a heightened sympathetic drive to the heart, potentially leading to heart palpitations.
Diagnosing Sleep Apnea and Heart Palpitations

The diagnosis of sleep apnea and heart palpitations is a two-step process. The first is polysomnography, a sleep study that monitors various physiological variables necessary for diagnosing sleep apnea and heart palpitations. This involves connecting the patient to equipment that monitors:
-
heart, lung, and brain activity
-
breathing patterns
-
limb movements
-
blood oxygen levels during sleep
Physiological variables such as EEG (brain waves), electro-oculogram (eye movements), electromyogram (muscle activity), electrocardiogram (heart activity), airflow, breathing efforts from the abdomen and thorax, snoring, body position, peripheral oxygen saturation, and heart rate are monitored during polysomnography.
The second step is an electrocardiogram (ECG/EKG), which is used to:
-
Assess heart rhythm
-
Detect abnormalities
-
Capture the heart’s electrical signal to detect various heart conditions
-
Assess heart function, including heart rate and rhythm
-
Identify irregularities
-
Aid in the diagnosis of heart disease.
Polysomnography
Polysomnography, commonly known as a sleep study, is a vital test for diagnosing sleep disorders such as sleep apnea and heart palpitations. It involves monitoring various physiological parameters during sleep, including:
-
Brain waves
-
Airflow
-
Respiratory effort
-
Oxygen levels
-
Heart rate
A technologist remains present during the test to diligently monitor and record the results, as well as to provide assistance in addressing any potential issues that may arise during the night.
Polysomnography is recognized for its significant diagnostic precision in identifying sleep apnea. It meticulously captures and analyzes various parameters such as:
-
Oximetry
-
Heart rate
-
Airflow
-
Respiratory effort
Polysomnography is crucial in the identification and efficient treatment of sleep apnea, a common sleep disorder, offering comprehensive insights into the presence and severity of the condition.
Electrocardiogram (ECG/EKG)
An electrocardiogram (ECG or EKG) records the heart’s electrical activity to identify a range of heart conditions. It is instrumental in assessing heart function, including:
-
Heart rate
-
Heart rhythm
-
Identifying irregularities
-
Aiding in the diagnosis of heart disease.
The EKG is a valuable tool for diagnosing sleep apnea and heart palpitations. It can:
-
Record the electrical activity of the heart
-
Analyze heart rate and cardio-respiratory coupling
-
Enable the detection of heart palpitations caused by sleep apnea.
Treatment Options for Sleep Apnea and Heart Palpitations

There are multiple treatment options for sleep apnea and heart palpitations. Some of these options include:
-
Continuous positive airway pressure (CPAP) therapy: This has been found to be effective in reducing the frequency of bradycardia episodes and may help reduce arrhythmias by improving oxygen supply.
-
Lifestyle changes: Weight loss can play a significant role in the treatment of sleep apnea and heart palpitations as it reduces the risk of atrial fibrillation, improves hypertension and diabetes management, and decreases upper airway collapsibility in sleep apnea.
-
Smoking cessation: Quitting smoking can enhance sleep quality by minimizing sleep disturbances and enhancing sleep efficiency, reducing the likelihood of severe cardiovascular disease events.
Other treatments may include medications and therapies to manage underlying medical conditions contributing to sleep apnea and heart palpitations. Beta blockers, including metoprolol, atenolol, nadolol, carvedilol, and acebutolol, are frequently recommended for the management of sleep apnea and heart palpitations.
Continuous Positive Airway Pressure (CPAP)
Continuous positive airway pressure (CPAP) therapy, a standard treatment for sleep apnea and heart palpitations, aids in keeping the airway open during sleep. CPAP treatment functions by enhancing the oxygen supply during sleep and diminishing the occurrence of bradycardia episodes to address sleep apnea and heart palpitations.
CPAP treatment has shown to significantly reduce heart rate variability during sleep, decrease sympathetic nervous system activity, and decrease the likelihood of heart-related complications, such as AFib. However, using CPAP may lead to various side effects including discomfort and skin irritation, claustrophobia, infections, nasal congestion, and dry nose, among others.
Lifestyle Changes
Making lifestyle changes can greatly impact the management of sleep apnea and heart palpitations. Obesity significantly contributes to the causal relationship between sleep apnea and cardiovascular disease. Both sleep apnea and obesity independently elevate the risk of health conditions that have adverse effects on heart health.
Smoking cessation can have a positive impact on sleep apnea by improving sleep quality and reducing the risk of heart palpitations and irregular heartbeats associated with smoking. Alcohol consumption can exacerbate the risk of sleep apnea and heart palpitations, and also elevate the probability of atrial fibrillation.
Medications and Therapies
Prescribed medications and therapies can help manage medical conditions that contribute to sleep apnea and heart palpitations. The medications typically prescribed for sleep apnea-induced heart palpitations may vary depending on the underlying cause and individual patient needs.
The use of anti-arrhythmic drugs is crucial in addressing heart palpitations associated with sleep apnea, as they play a key role in decreasing the likelihood of atrial fibrillation recurrence following rhythm control interventions. Blood pressure medications, such as beta-blockers, play a supportive role in managing sleep apnea and heart palpitations by regulating heart rate increases caused by apneas during sleep.
Preventive Measures for Sleep Apnea and Heart Palpitations
Prevention of sleep apnea and heart palpitations involves good sleep hygiene practices and stress management through relaxation techniques and exercise. Adhering to a consistent sleep schedule can potentially aid in preventing sleep apnea and heart palpitations by establishing a regular routine, thereby reducing stress levels, managing stimulant intake closer to bedtime, and promoting overall healthy sleep patterns.
Sleep Hygiene
Maintaining good sleep hygiene is crucial in preventing sleep apnea and heart palpitations. This includes establishing regular sleep routines, creating a conducive sleep environment, and effectively managing stress before bedtime.
Some habits to foster undisturbed sleep include:
-
Adhering to a consistent sleep schedule
-
Refraining from stimulants such as caffeine and alcohol near bedtime
-
Ensuring a gap of at least two hours between eating and bedtime
Stress Management
Managing stress is also vital in preventing sleep apnea and heart palpitations. Relaxation techniques such as yoga, meditation, and deep breathing exercises not only aid in reducing stress but can also assist sleep apnea patients in falling asleep more easily and have a better experience with CPAP treatment for treating sleep apnea.
Regular physical activity has a beneficial effect on preventing sleep apnea by:
-
improving autonomic nervous function
-
reducing the severity of apnea events
-
reducing the stress on the heart, potentially decreasing the likelihood of experiencing heart palpitations and disorders such as arrhythmia.
Summary
In conclusion, sleep apnea, a disorder characterized by interrupted breathing during sleep, can lead to heart palpitations due to changes in intrathoracic pressure, sympathetic and parasympathetic system activation, and myocardial ischemia. There are several risk factors for developing sleep apnea and heart palpitations, including lifestyle factors such as obesity, smoking, and alcohol consumption, as well as medical conditions like hypertension, diabetes, and metabolic syndrome.
It’s crucial to recognize the symptoms of sleep apnea-induced heart palpitations and seek medical attention if you experience them. Treatment options include continuous positive airway pressure (CPAP) therapy, lifestyle changes, and medications or therapies to manage underlying medical conditions. Preventive measures include practicing good sleep hygiene and managing stress through relaxation techniques and exercise. Remember, early detection and treatment can significantly improve your quality of life and reduce the risk of severe complications.
Frequently Asked Questions
Will CPAP help with heart palpitations?
Yes, CPAP therapy has been shown to be effective in reducing cardiac arrhythmias and improving heart health in patients with sleep apnea. It can help reduce arrhythmias by improving oxygen supply while you sleep.
Can sleep problems cause heart palpitations?
Yes, poor sleep can lead to increased heart rate and irregular heartbeat, which may cause heart palpitations.
Is there a relationship between sleep apnea and cardiac arrhythmias?
Yes, there is a relationship between sleep apnea and cardiac arrhythmias. Studies suggest a high prevalence of cardiac arrhythmias in patients with obstructive sleep apnea (OSA) and vice versa, and OSA may contribute to arrhythmias due to various mechanisms.
Why am I waking up with heart palpitations?
It's common to wake up with heart palpitations due to stress, sleep deprivation, sleep apnea, and changes in blood sugar levels, which can lead to a racing heart, shakiness, or anxiety.
Symptoms of sleep apnea?
Symptoms of sleep apnea include: Obstructive sleep apnea includes...