What is obstructive sleep apnea (OSA), and why is it critical to recognize and treat it? This sleep disorder not only disrupts your night but can also pose severe health risks without proper management. Our guide offers an in-depth look at detecting OSA’s symptoms, understanding its causes, and reviewing effective treatment options.
Key Takeaways
-
Obstructive Sleep Apnea (OSA) is characterized by repeated episodes of partial or complete upper airway obstruction during sleep, leading to disturbed sleep, health complications like cardiovascular disease, and an increased risk of accidents.
-
OSA symptoms manifest as loud snoring, observed episodes of stopped breathing at night and excessive daytime sleepiness. Risk factors include obesity, smoking, alcohol, sedatives, and certain medical conditions.
-
Treatment options for OSA vary from lifestyle modifications and Continuous Positive Airway Pressure (CPAP) therapy to oral appliances and surgical interventions, with treatment choices often based on OSA severity and individual patient needs.
Understanding Obstructive Sleep Apnea

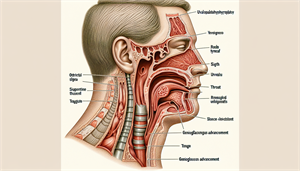
OSA is a sleep disorder distinguished by occurrences of upper airway collapse while sleeping, resulting in sleep disordered breathing, disturbed sleep, and potential health issues. Imagine a garden hose with water flowing freely. Now, picture someone stepping on that hose, obstructing the flow of water. This is what happens in OSA when the upper airway collapses, obstructing the flow of air and thereby fostering the onset of obstructive sleep apnea syndrome (OSA).
This interference with normal breathing can lead to various health complications, including:
-
Daytime sleepiness
-
Mood changes
-
High blood pressure
-
Cardiovascular disease
Even daily activities such as driving can become risky, as individuals with severe OSA demonstrate a heightened probability of being engaged in motor vehicle accidents.
Keep in mind, not every type of sleep apnea is the same. OSA is just one variant among many. So, how does it differ from the others?
How OSA occurs
Imagine trying to drink a thick milkshake through a tiny straw. You suck in, but the milkshake doesn’t budge—the straw is just too narrow. This is similar to what happens in OSA. During sleep, the relaxation of throat muscles can result in the closure of airway tissues, leading to the narrowing or collapse of the pharyngeal airway. In response, the body increases blood pressure and triggers brief awakenings, known as arousals or microarousals, to reopen the airway. These disruptions in sleep can lead to a decrease in blood oxygen levels and can occur even in cases of mild sleep apnea.
One might wonder, how does OSA stand out from other forms of sleep apnea?
Differentiating OSA from central and complex sleep apnea
While OSA is distinguished by the physical obstruction of the airway causing breathing pauses, central sleep apnea (CSA) is marked by the absence of respiratory effort due to inadequate signals from the brain to the muscles controlling breathing. Unlike OSA, CSA is often linked to severe conditions affecting the lower brainstem or to underlying medical issues such as congestive heart failure or stroke. In some cases, individuals may experience symptoms of both OSA and CSA, a condition known as complex sleep apnea syndrome (CompSAS).
How can one identify if they or someone close to them has OSA? Let’s explore the symptoms and warning signs.
Symptoms and Warning Signs

If OSA were a movie villain, it would be the kind that lurks in the shadows, revealing its presence through subtle signs. Typical symptoms of severe sleep apnea encompass excessive daytime sleepiness, loud snoring, and instances of gasping, choking, or breathing cessation observed by a bed partner during sleep. Consider experiencing a day overwhelmed with excessive tiredness, grappling with morning headaches, and waking up to a dry mouth or sore throat. These are some of the specific daytime symptoms that may indicate the presence of Obstructive Sleep Apnea.
While these symptoms may seem straightforward, they can manifest differently during the night and the day. The nighttime severe obstructive sleep apnea symptoms encompass loud snoring, observed episodes of stopped breathing, and waking during the night, while the daytime symptoms consist of excessive daytime sleepiness and fatigue. What could be the possible causes for this condition?
Nighttime symptoms
As the moon rises and the world prepares for slumber, the stage is set for OSA to make its appearance. The loud snoring in obstructive sleep apnea is primarily attributed to:
-
the partial blockage or narrowing of the airway during sleep, leading to the vibration of throat tissues and the characteristic sound of snoring
-
interruptions in breathing that can last from 10 seconds to one minute or longer
-
choking or gasping episodes that often accompany the interruptions
These episodes are a silent battle, as the body fights to breathe amidst the obstruction.
What occurs when daylight breaks?
Daytime symptoms
The battle with OSA doesn’t end with the break of dawn. Daytime brings its own set of challenges. Excessive daytime sleepiness caused by OSA results from inadequate restorative sleep during the night, leading to:
-
fatigue
-
sleepiness
-
cognitive function impairment
-
mood changes
Moreover, despite having slept for a full duration, individuals with OSA often report feeling tired or exhausted, a state known as nonrestorative sleep. While it’s evident that OSA influences more than just sleep, what triggers it?
Risk Factors and Causes

Like a villain with a band of accomplices, OSA doesn’t act alone. It often has allies in the form of lifestyle-related risks and medical conditions. These include:
-
Obesity
-
Smoking
-
Alcohol consumption
-
Use of sedatives
These factors can all increase the likelihood of developing obstructive sleep apnea. Obesity, in particular, plays a significant role in OSA by exerting elevated pressure on the upper airways, making them more prone to collapse during sleep. However, the risk factors for OSA aren’t limited to lifestyle choices.
Lifestyle-related risks
Let’s delve deeper into the role of lifestyle in OSA. Obesity plays a significant role in OSA by decreasing the size of the airway, making it more prone to collapse during sleep. Moreover, smoking can increase the risk of OSA by inducing relaxation in the upper airway muscles, potentially resulting in airway obstruction during sleep. Even alcohol consumption can have a notable impact on the severity of OSA, disrupting the sleep architecture and worsening breathing challenges during sleep.
What about the influence of medical conditions?
Medical conditions and OSA
Medical conditions can also join forces with OSA. Certain medical conditions can lead to nasal congestion and blockage, increasing the risk of developing sleep apnea. Genetics, too, can have a role in the likelihood of developing obstructive sleep apnea through factors such as oxidative stress.
Given these potential risk factors, how do healthcare professionals approach the diagnosis of OSA?
Diagnosis and Evaluation
Diagnosing OSA involves piecing together a multitude of signs, symptoms, and test results. Central to this process are sleep studies, which monitor and assess an individual’s breathing and other physiological functions during sleep. These studies confirm the existence of OSA and assess its severity. The diagnostic process often includes:
-
A comprehensive physical examination
-
A thorough review of symptoms and medical history
-
Chest radiography
-
Electrocardiography
-
Echocardiography
-
Overnight polysomnography
These tests help healthcare professionals accurately diagnose OSA and develop an appropriate treatment plan.
The role of sleep studies
Sleep studies serve as the cornerstone for diagnosing OSA. They provide a detailed picture of what happens in your body during sleep. Polysomnography, for example, is a comprehensive sleep study that monitors various physiological parameters during sleep to evaluate for OSA.
Home sleep apnea testing (HSAT) offers a convenient, less invasive alternative, enabling patients to undergo testing in the comfort of their own homes using devices that can measure heart rate, breathing, and other pertinent data for OSA diagnosis. How can these results be deciphered?
Interpreting sleep study results
Interpreting sleep study results is like reading a map of your sleep. It involves analyzing the number of complete pauses in breathing (apneas) and partial reductions in breathing (hypopneas) during sleep, using the apnea-hypopnea index (AHI). Oxygen desaturation levels are also evaluated, as they indicate the frequency of low blood oxygen levels during sleep, often quantified by the oxygen desaturation index (ODI), and reflect episodes of significant breathing disruption.
Once obstructive sleep apnea diagnosed, how is obstructive sleep apnea treated and managed?
Treatment Options for Obstructive Sleep Apnea

Treating OSA involves a multifaceted approach, that can include lifestyle modifications, medical interventions, and even surgical procedures. One way to treat obstructive sleep apnea is through Continuous Positive Airway Pressure (CPAP) therapy, which involves the use of a machine that delivers air pressure through a mask to keep the airway open during sleep. This is generally considered the most effective treatment for mild to severe OSA. Nevertheless, it’s not the sole option available.
Lifestyle modifications
Lifestyle modifications can play a pivotal role in managing OSA. Weight loss, for instance, can alleviate symptoms of OSA, including daytime sleepiness and irritability. Additionally, mouth and throat exercises, such as tongue protrusion and tongue slides, have shown effectiveness for individuals with OSA.
Nonetheless, certain lifestyle factors like the use of sedatives can aggravate OSA symptoms, which is one of the common sleep disorders.
Positive airway pressure therapies
Positive airway pressure therapies, such as CPAP, serve as powerful allies in the battle against OSA. By delivering a constant flow of air pressure through a mask, they keep the airway open and prevent its collapse during sleep.
With continuous updates and improvements in CPAP technology, newer devices are lighter, quieter, and more comfortable compared to older models, making them a popular choice for treating OSA.
Oral appliances and alternative treatments
For those who cannot tolerate CPAP therapy, oral appliances and alternative treatments can offer a viable solution. Some options include:
-
Oral appliances, which function by adjusting the position of the jaw or tongue to uphold an unobstructed airway
-
Positional therapy, which promotes sleep positions that mitigate airway collapse and offers particular benefit to individuals with position-dependent obstructive sleep apnea
-
Medical or surgical interventions, which may be required in certain situations
Surgical Interventions
When lifestyle changes and medical treatments fail to manage OSA, surgical interventions may be considered as a last resort. These can include:
-
Removal of tonsils, adenoids, or excessive tissue in the throat or nasal passages
-
Jaw reconstruction to widen the upper airway
-
Insertion of plastic rods into the soft palate
Indications for surgery
The decision to proceed with surgical intervention in OSA is typically influenced by the severity of the condition, the effectiveness of non-surgical treatments, and specific anatomical factors contributing to the obstruction. Surgical options, such as tongue reduction and uvulectomy, may be evaluated, with diagnostic tools and algorithms commonly utilized to assess the patient’s candidacy for surgery.
Potential risks and complications
Like any surgical procedure, interventions for OSA carry potential risks and complications. These can encompass perioperative morbidity, postoperative oxygen desaturation, delirium, and even wound breakdown. Post-surgical infections, such as hospitalization-associated EV infection and surgical site infection, are commonly addressed with antibiotic therapy, and in certain instances, management may involve oxygen therapy and ventilatory monitoring in conjunction with proper wound care to mitigate additional complications.
Nevertheless, it’s vital to remember that OSA isn’t exclusive to adults.
Obstructive Sleep Apnea in Children
OSA doesn’t discriminate by age. It can also affect children, presenting with symptoms such as snoring, restless sleep, and daytime sleepiness, and impacting their growth and learning. In children, the predominant factors contributing to OSA are often enlarged tonsils and adenoids.
Identifying OSA in children
Identifying OSA in children involves recognizing typical symptoms such as snoring, pauses in breathing, and restless sleep. OSA can also impact a child’s behavior, potentially leading to attention deficit, disruptive behaviors, hyperactivity, and even bed-wetting.
The impact of OSA on a child’s growth and cognitive development can be significant, making early diagnosis and treatment crucial.
Treatment options for pediatric OSA
Just as in adults, the treatment of OSA in children requires a multifaceted approach. For children with OSA resulting from enlarged tonsils and adenoids, the recommended course of treatment is often an adenotonsillectomy procedure. Measures such as weight loss and lifestyle modifications can also assist children with OSA stemming from excess weight.
In some cases, CPAP therapy may also be indicated.
Summary
From the subtle signs and symptoms, through the complex diagnostic process, to the variety of treatment options, we’ve journeyed through the fascinating world of OSA. It’s clear that understanding OSA is crucial, not just for those who are affected, but also for their loved ones and healthcare providers. While the path may seem challenging, armed with knowledge and guided by specialists, overcoming OSA is possible. Remember, every breath counts.
Frequently Asked Questions
Can you fix sleep apnea?
Yes, lifestyle changes such as weight loss, regular physical activity, and quitting smoking and drinking can improve mild cases of sleep apnea, but CPAP therapy is still the gold standard for treatment.
What is the best medication for sleep apnea?
The best medications for sleep apnea include acetazolamide, modafinil, and armodafinil. These medications can help manage breathing and improve symptoms of obstructive and central sleep apnea.
What is the cause of obstructive sleep apnea?
The cause of obstructive sleep apnea is the relaxation of muscles in the throat combined with a narrowed airway, which interrupts breathing during sleep. Factors like excess weight, obesity, large tonsils, and changes in hormone levels can increase the risk of this condition.
How is OSA diagnosed?
OSA is diagnosed through a comprehensive process involving symptom review, medical history, physical examination, and often a sleep study, such as polysomnography. A thorough assessment is essential to accurately diagnose OSA.
Can children have OSA?
Yes, children can have obstructive sleep apnea (OSA), which may present as symptoms like snoring, restless sleep, and daytime sleepiness, and can affect their growth and learning.


