Imagine being jolted awake repeatedly, gasping for breath, night after night. This is the reality for those suffering from sleep apnea, a prevalent but frequently overlooked sleep disorder. But, the good news is that with the right knowledge and proactive actions, it’s entirely manageable.
So, let’s unravel the enigma of sleep apnea together, from understanding its nature to exploring how to test for sleep apnea at home.
Key Takeaways
-
Sleep apnea is a potentially serious sleep disorder that occurs when a person’s breathing is interrupted during sleep, with two primary types being obstructive sleep apnea (OSA) and central sleep apnea (CSA), each with its own causes and implications for health.
-
Diagnosis of sleep apnea involves recognizing symptoms, consulting a sleep specialist who considers both symptoms and medical history, and may recommend an in-lab polysomnography or at-home sleep test based on the initial assessment.
-
Treatment options for sleep apnea include lifestyle changes and medical interventions like CPAP therapy, which involves using a machine to ensure continuous airflow during sleep, with ongoing treatment management and monitoring being crucial.
Understanding Sleep Apnea
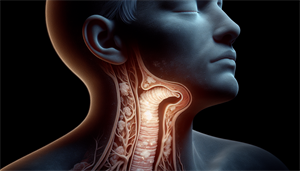
Sleep apnea is a sleep disorder characterized by recurrent closure or constriction of the airway during the night, leading to restricted airflow and oxygen supply. The two primary types of sleep apnea are obstructive sleep apnea (OSA), which involves physical obstruction of the airway, and central sleep apnea (CSA), wherein the brain inadequately regulates breathing during sleep. The physical obstruction in OSA could be due to the collapse of surrounding tissues such as the tongue, uvula, tonsils, or soft palate, leading to airway blockage during sleep.
Indeed, adult obstructive sleep apnea is a chronic condition that requires continuous care to prevent health complications. Untreated severe obstructive sleep apnea can lead to significant health concerns such as:
-
Cardiovascular complications
-
Elevated blood pressure
-
Risk of stroke
-
Potential development of depression
All of these health concerns, including other sleep disorders, are linked to disrupted breathing patterns during sleep.
Identifying the Need for Sleep Apnea Testing

The first step towards diagnosing and treating sleep apnea is recognizing its symptoms. Typical indicators of sleep apnea encompass daytime sleepiness, snoring, and morning headaches, which may necessitate further assessment for sleep apnea such as home sleep apnea testing or in-lab sleep studies. Don’t ignore these signs. If you observe these symptoms, seek advice from a healthcare provider on sleep apnea to determine if testing is necessary.
Certain individuals, due to specific personal traits or family history, as well as those with particular health conditions such as cardiac conditions, are at a heightened risk for sleep apnea and should consider undergoing testing. Testing and diagnosis of sleep apnea are critical, as untreated sleep apnea could lead to serious physical and mental health problems.
Consultation with a Sleep Specialist
Meeting with a sleep specialist is an important step to diagnose sleep apnea. During the initial consultation, a sleep specialist may inquire about symptoms such as excessive daytime sleepiness, loud snoring, and episodes of gasping for air while asleep to assess whether a patient should be recommended for a sleep study. The sleep specialist also takes into consideration the patient’s personal and family medical history, which can indicate a higher risk of sleep apnea.
Based on the initial assessment of symptoms, physical examination, and evaluation of personal and family medical history, a sleep specialist might advise a sleep study if they indicate a potential for sleep apnea.
Initial Assessment
During the initial assessment, a sleep specialist conducts a physical examination, which includes considering a patient’s weight, neck circumference, and blood pressure to assess their risk of sleep apnea. The sleep specialist will also inquire about a range of symptoms related to sleep patterns, such as the severity of snoring, frequency of nighttime awakenings, and feelings of restlessness or fatigue during the day.
Besides the physical examination, the assessment includes:
-
A comprehensive review of the patient’s personal and family medical history
-
The patient may be asked to complete a questionnaire regarding their sleep habits
-
A conversation about any pertinent personal and family medical history related to sleep apnea will be conducted.
Sleep Study Recommendation
Based on the initial assessment, a sleep specialist may recommend a sleep study. If the doctor suspects sleep apnea based on the patient’s examination and symptoms, they are inclined to suggest that the patient undergo a sleep study to obtain an accurate diagnosis. The decision to recommend a sleep study is not taken lightly. Sleep specialists take into account a range of factors such as:
-
observed gasping during sleep
-
morning headache
-
excessive daytime sleepiness
-
loud snoring
-
obesity
-
high blood pressure
-
other sleep apnea risk factors
The type of sleep study recommended depends on the patient’s symptoms and sleep history. In-lab sleep studies are typically suggested for more thorough assessments, intricate cases, or when there are suspicions of additional sleep disorders. On the other hand, at-home sleep tests may be used for convenience and cost-efficiency in evaluating obstructive sleep apnea.
Types of Sleep Apnea Tests

Having established the need for sleep apnea tests and their recommendation methods, we will now discuss the different types of sleep apnea tests. The two primary types of tests are in-lab polysomnography and at-home sleep apnea tests. In-lab polysomnography, also referred to as a Type 1 sleep apnea test, is a thorough sleep study used for diagnosing sleep apnea. It includes the use of multiple monitors to track brain waves, body movement, airflow, and other physiological data.
On the other hand, the main types of at-home sleep apnea tests are the Type 2 test and the Type 4 test. These tests are more convenient and cost-effective but may be potentially less accurate.
In-Lab Polysomnography
In-lab polysomnography is conducted in a sleep lab by a qualified sleep technician. It involves the use of multiple monitors to track:
-
brain waves
-
body movement
-
airflow
-
other physiological data
This test provides a comprehensive overview of your sleep patterns and can even involve the use of continuous positive airway pressure (CPAP) therapy if sleep apnea is detected during the study.
Preparation for in-lab polysomnography includes several steps. Before the test, it’s recommended to:
-
Avoid using lotions, gels, colognes, or makeup
-
Follow any bathing and grooming guidelines provided by your healthcare provider
-
Consult them about medication usage before the test
At-Home Sleep Apnea Tests

At-home sleep apnea tests are a more convenient and affordable alternative to in-lab polysomnography. These tests involve wearing a portable breathing monitor overnight to detect and measure pauses in breathing, referred to as apneas, as well as monitoring blood oxygen levels. The severity of obstructive sleep apnea is assessed by determining the average occurrences of breathing pauses per hour during sleep.
To conduct an at-home sleep apnea test, it’s important to prepare the bedroom in a manner that promotes a comfortable sleep environment. The test should be conducted at your usual bedtime to replicate your typical sleep routine.
Following the test, a sleep medicine specialist evaluates the data and collaborates with you to determine the most suitable treatment plan. In cases of persistent symptoms or inconclusive results, an in-lab study may be recommended.
Preparing for Your Sleep Apnea Test
Whether preparing for an in-lab sleep study or an at-home sleep apnea test, consider a few things. One recommendation is to arrange your sleep environment to promote a comfortable sleep. This includes wearing comfortable pajamas and setting up your bedroom to replicate your typical sleep routine.
Before an in-lab polysomnography test, it’s advisable to:
-
Refrain from using lotions, gels, colognes, or makeup
-
Adhere to any bathing and grooming recommendations provided by your healthcare provider
-
Consult with them regarding the usage of medications before the test.
Interpreting Sleep Apnea Test Results
After completing your sleep apnea test, the subsequent step involves interpreting the results. The Apnea-Hypopnea Index (AHI) is used to determine the presence and severity of sleep apnea. The AHI represents the average number of apneas and hypopneas that occur per hour of sleep. Sleep apnea is considered present if there are at least 5 breathing events per hour of sleep.
The severity of sleep apnea is categorized based on the AHI levels as:
-
None/minimal (AHI < 5 per hour)
-
Mild (AHI ≥ 5, but < 15 per hour)
-
Moderate (AHI ≥ 15, but < 30 per hour)
-
Severe (AHI ≥ 30 per hour)
Along with the AHI, the sleep specialist at the sleep center will also consider your symptoms and medical history to determine the most suitable treatment options.
Treatment Options for Sleep Apnea

After being diagnosed with sleep apnea, the next step involves examining treatment options. Treatment options range from lifestyle changes, such as weight loss, regular exercise, cessation of alcohol and tobacco use, to more medical interventions, such as continuous positive airway pressure (CPAP) therapy.
CPAP therapy is a widely utilized and efficient method for addressing sleep apnea. It involves a machine that delivers a continuous flow of pressurized air through a mask, which helps keep the airway open during sleep. This treatment not only prevents airway collapse but also alleviates sleep apnea symptoms, ensuring uninterrupted breathing throughout the night.
Monitoring and Managing Sleep Apnea
After starting treatment, continual monitoring and management of your sleep apnea is advised. Regular follow-up consultations at least once after starting CPAP treatment and at least yearly thereafter are recommended to ensure proper management of the condition.
Moreover, lifestyle adjustments play a pivotal role in managing sleep apnea. These include:
-
Weight loss
-
Increased physical activity
-
Abstaining from alcohol and tobacco
-
Avoiding specific medications
-
Altering sleep positions to enhance breathing
These adjustments can help improve symptoms and overall sleep quality.
Summary
We’ve journeyed together through understanding sleep apnea, identifying its symptoms, consulting with a sleep specialist, exploring various testing options, preparing for a sleep test, interpreting the results, and finally, discussing treatment options and how to monitor and manage the condition. Remember, sleep apnea is not just a disruptor of sleep but, if left untreated, can lead to serious health conditions. Therefore, it’s imperative to take proactive steps if you suspect you have sleep apnea.
Frequently Asked Questions
Can I test myself for sleep apnea?
Yes, you can test yourself for sleep apnea using at-home sleep apnea testing, which is a cost-effective and simplified way to monitor your breathing and oxygen levels. This can help you determine if you're experiencing trouble breathing during sleep.
How do doctors check for sleep apnea?
Doctors check for sleep apnea through a polysomnogram, also known as a sleep study, which involves monitoring various body activities and breathing patterns while the patient sleeps. This can be conducted in a lab or at home and is considered the gold standard for diagnosis.
What are 3 symptoms of sleep apnea?
Common symptoms of sleep apnea include feeling tired or exhausted upon waking, daytime sleepiness, and snoring. These may also be accompanied by mood changes and disruptions in brain function.
Can sleep apnea be cured without CPAP?
Non-CPAP options such as lifestyle changes and fitted mouthpieces can help with mild sleep apnea, but for moderate to severe cases, these alternatives are rarely successful.
What is the difference between in-lab and at-home sleep apnea tests?
In-lab sleep apnea tests are conducted in a sleep lab and monitor a variety of physiological data, while at-home tests are more convenient and cost-effective but may be less accurate. Ultimately, the choice depends on various factors, including the individual's preferences and the severity of the sleep apnea.


