People searching for ‘covid and sleep apnea’ are often seeking to understand the connection between the respiratory virus and sleep-related breathing disorders. This article dives directly into how sleep apnea can complicate COVID-19 infections, the heightened risks, and what protective measures or treatment approaches can be taken. Gain clear, concise knowledge on managing these intertwined health challenges.
Key Takeaways
-
Obesity, hypertension, and other comorbidities are shared risk factors that can exacerbate the severity of both COVID-19 and obstructive sleep apnea (OSA), leading to complications such as hypoxemia.
-
Sleep apnea can potentially increase the severity of COVID-19 by worsening respiratory symptoms and elevating levels of inflammatory cytokines, thereby intensifying the inflammatory response during infection.
-
Continuous Positive Airway Pressure (CPAP) machines, commonly used for treating sleep apnea, raise concerns about virus transmission during the COVID-19 pandemic, yet proper precautions can minimize risks and CPAP therapy may alleviate respiratory distress caused by COVID-19.
The Interplay Between COVID-19 and Obstructive Sleep Apnea
Navigating the labyrinth of COVID-19 and obstructive sleep apnea uncovers a world where risk factors and comorbidities intermingle. Obesity, hypertension, and chronic obstructive pulmonary disease often act as unwelcome companions for both COVID-19 and OSA patients, potentially worsening each other’s effects on the body.
The common ground shared by these conditions forms a perilous landscape for patients, with the potential to exacerbate hypoxemia seen in COVID-19 pneumonia. This complex interplay may serve as an obstructive sleep apnea lead, guiding researchers and clinicians in understanding and managing these interconnected health issues.
Understanding these comorbidities is vital as they shed light on potential pathophysiological mechanisms that can influence outcomes in patients with sleep disordered breathing, such as OSA. It’s like a riddle wrapped in a mystery inside an enigma; but perhaps with further research, we might find the key.
Common Risk Factors
Obesity emerges as a common adversary in the intersection of COVID-19 and OSA. Patients with both COVID-19 and OSA have a significantly high prevalence of obesity, which increases the risk of developing OSA and can lead to adverse health outcomes. It’s a vicious cycle, where one condition fuels the other, creating a health crisis of enormous proportions.
Yet, the narrative extends beyond obesity. Hypertension and diabetes also join the battle, each intensifying the severity of both COVID-19 and OSA. It’s like a domino effect, where one condition sets off a chain reaction, exacerbating the other. These risk factors, including obesity and diabetes, act as catalysts, accelerating the severity of both conditions. It’s a stark reminder that when it comes to COVID-19 and OSA, it’s not just about battling a single foe, but an entire army of risk factors.
Comorbidities
While risk factors set the stage for the onset of COVID-19 and OSA, comorbidities often play a starring role in their progression. Cardiovascular disease and respiratory issues, in particular, often wear the villain’s mask in this narrative, exacerbating the increased risk and severity of both conditions. A single risk factor may not be solely responsible, as other risk factors may also contribute to the overall health impact.
When it comes to cardiovascular diseases, the impact on OSA patients is significant. Patients with OSA often have a prevalence of cardiovascular diseases ranging from 40% to 80%, encompassing conditions such as hypertension, heart failure, and coronary artery disease.
On the other hand, COVID-19 has the potential to exacerbate symptoms in individuals with pre-existing cardiovascular conditions, leading to increased occurrences of chest pain and shortness of breath. It’s a precarious situation that requires careful management to ensure that these comorbidities do not tip the scales towards more severe outcomes.
How Sleep Apnea Affects COVID-19 Severity

Beyond the grim picture painted by the shared risk factors and comorbidities of COVID-19 and OSA, the influence of sleep apnea on COVID-19 severity introduces a new layer of complexity. OSA can exacerbate respiratory symptoms in COVID-19 patients, potentially resulting in heightened hospitalization rates and severe outcomes. Additionally, OSA is linked to heightened levels of inflammatory cytokines, which may play a role in intensifying the inflammatory response during a COVID-19 infection. It’s like a thunderstorm brewing on the horizon, with sleep apnea acting as the dark clouds that could potentially unleash a downpour of complications.
Impact on Respiratory System
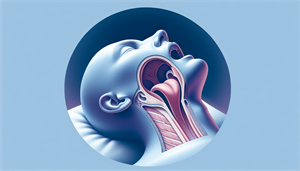
If we think of our lungs as the engine that keeps us running, adult obstructive sleep apnea (OSA) could be likened to a wrench thrown into the gears. By causing periodic cessation of breathing during sleep, OSA results in intermittent reductions in airflow to the lungs and fluctuations in oxygen levels, leading to airway obstruction. It’s like trying to breathe through a straw, only to have it pinched off intermittently. This condition, also known as sleep apnoea, can have serious consequences for those affected by it.
When COVID-19 enters the fray, the situation becomes even more perilous. The virus could worsen respiratory issues in OSA patients, contributing to endothelial dysfunction, increasing the risk of infection, and impairing already compromised respiratory function, which can lead to exacerbation of breathing difficulties, sleep problems, and fatigue. Thus, OSA and COVID-19 together could create a perfect storm of respiratory distress, leading to heightened hospitalization rates and increased severity of COVID-19 outcomes.
Inflammatory Response
While the impact of OSA on the respiratory system is evident, its influence on the body’s inflammatory response adds another dimension to this complex narrative. Inflammatory cytokines such as IL-6, which play a vital role in the immune response to COVID-19, are often elevated in OSA patients. It’s like a fire alarm going off in the body, signaling the existence and extent of inflammation.
The mechanisms through which OSA increases IL-6 levels in the body are linked to sleep deprivation and hypoxemia, both caused by the recurrent airway collapse and obstruction characteristic of OSA. Elevated IL-6 levels have been associated with heightened severity of COVID-19, showing a correlation with disease stages, radiologic changes, and an increased likelihood of disease progression. Thus, the inflammatory response in OSA patients could potentially fan the flames of COVID-19, leading to a more severe disease course.
Long COVID and Sleep Apnea: A Vicious Cycle

As we delve deeper into the relationship between COVID-19 and sleep apnea, we come across the specter of long COVID. Coexisting with sleep apnea, long COVID can potentially worsen the symptoms of the disease, creating a vicious cycle that can lead to persistent symptoms and impact mental health.
It’s like being trapped in a maze where every turn leads back to the start, with the symptoms of long COVID and OSA feeding off each other.
Persistent Symptoms
The symptoms of long COVID, such as fatigue, cognitive impairment, and sleep disturbances, echo the persistent symptoms often seen in OSA patients. It’s like looking in a mirror and seeing a reflection that’s all too familiar, with the symptoms of long COVID mirroring those of OSA.
This overlap of symptoms can pose challenges in the recovery process. For instance, the prevalence of cognitive impairment in long COVID patients varies widely, raising concerns due to the comparable cognitive difficulties experienced by many individuals with OSA. It’s a tangled web of symptoms, making the journey to recovery a challenging one.
Impact on Mental Health
While the physical symptoms of long COVID and OSA are in the spotlight, the mental health impact of both conditions often lurks in the shadows. Both long COVID and sleep apnea have the potential to result in notable mental health challenges, such as:
-
depression
-
anxiety
-
cognitive decline
-
an elevated susceptibility to suicidal ideation and attempts
These challenges further complicate the recovery process.
The mental health impacts of long COVID encompass depression, anxiety, fatigue, sleep disturbances, psychosis, cognitive impairment, and brain fog. Similarly, OSA impacts cognitive decline by chronically fragmenting sleep, leading to disruptions in memory consolidation, brain plasticity, and cerebral metabolic waste clearance. It’s a double-edged sword, with both conditions potentially contributing to significant mental health challenges and cognitive decline.
Managing Sleep Apnea During a COVID-19 Infection
For individuals with sleep apnea, managing a COVID-19 infection can feel like navigating through choppy waters. Diligent monitoring of symptoms and adjusting sleep apnea treatment as needed can be crucial in managing the condition during a COVID-19 infection.
Monitoring Symptoms
Given the multitude of symptoms associated with both COVID-19 and OSA, it becomes essential to effectively monitor symptoms. Individuals can observe and document a range of symptoms, including:
-
Cough
-
Fever
-
Chronic pain
-
Intense sleepiness
It’s like being a detective at the national center, piecing together the clues to better manage the conditions.
However, recognizing the signs is only half the battle. The real test lies in seeking immediate medical attention if COVID-19 symptoms worsen. Difficulty breathing, persistent chest pain or pressure, and sudden confusion are all signals that should not be ignored. It’s a battle that requires vigilance, courage, and prompt action to inform clinical care.
Sleep Apnea Treatment and COVID-19
Not only is symptom monitoring vital in managing sleep apnea during a COVID-19 infection, but adjusting the treatment for sleep apnea is of equal importance. The use of sleep apnea treatment apparatus, particularly CPAP machines, has raised concerns about virus transmission. However, regular and thorough cleaning of the equipment and maintaining good hand hygiene can go a long way in reducing these risks.
Furthermore, the use of a CPAP device may have the potential to mitigate the exacerbation of COVID-19 symptoms, but further research is required to validate its effect on disease severity. It’s like navigating uncharted territory, where every step forward can bring us closer to understanding the optimal way to manage sleep apnea during a COVID-19 infection.
CPAP Usage and COVID-19 Concerns
During the COVID-19 pandemic, several questions have arisen regarding the use of Continuous Positive Airway Pressure (CPAP) machines, a common treatment for sleep apnea. The primary concerns revolve around the safety of its use during an active COVID-19 infection and the potential impact on disease severity.
Safety of CPAP Use
On the surface, the use of CPAP machines during a COVID-19 infection might seem like a cause for concern. However, with appropriate precautions, it’s generally considered safe to continue using a CPAP device during the COVID-19 pandemic. It’s like driving a car – as long as you follow the safety rules and guidelines, the risks can be minimized.
These precautions include:
-
Regular cleaning of the CPAP equipment with mild soap and warm water
-
Properly rinsing the humidifier tub
-
Practicing good hand hygiene and social distancing to reduce the risk of virus transmission
It’s a comprehensive approach, where every small step contributes to ensuring the safe use of CPAP machines during a COVID-19 infection.
Potential Impact on Disease Severity
While the safety of CPAP usage during COVID-19 is of prime importance, it’s equally crucial to consider its potential impact on disease severity. There is some evidence to suggest that consistent use of a CPAP device may alleviate some of the respiratory distress caused by COVID-19, although more research is needed to validate this.
The existing evidence regarding the influence of CPAP therapy on the severity of COVID-19 in OSA patients is varied. Some studies suggest that adherent CPAP users may have a reduced likelihood of experiencing severe COVID-19 outcomes, while others haven’t found a clear association. It’s a puzzle that still needs to be solved, offering hope for a potential tool in our arsenal against COVID-19.
Seeking Medical Care for Sleep Apnea and COVID-19
Amid the complexities of COVID-19 and sleep apnea, the importance of seeking medical care for both conditions becomes evident for the correct diagnosis and treatment. Adhering to the general protocols for seeking medical care during the COVID-19 pandemic and following specific instructions from healthcare providers, such as those from a sleep medicine specialist like a clin sleep med expert, can help ensure optimal management of both conditions.
COVID-19 Medical Care
Timeliness is of the essence when dealing with COVID-19 medical care. COVID-19 symptoms can worsen rapidly, particularly in individuals with sleep apnea and other comorbidities, making immediate medical attention vital. It’s like a ticking time bomb, where every second counts.
However, the presentation of COVID-19 in patients with sleep apnea can vary, with symptoms often being more pronounced than in those without sleep apnea. Recognizing these differences and watching out for emergency signals such as difficulty breathing and persistent chest pain is crucial. It’s a delicate dance between vigilance and prompt action, one that can potentially save lives.
Sleep Apnea Medical Care
Parallel to the importance of COVID-19 medical care, the role of sleep apnea medical care is crucial in managing the condition and possibly lessening COVID-19 risks. Proper sleep apnea treatment, like CPAP therapy, can address sleep apnea symptoms and enhance respiratory health, potentially aiding in the management of COVID-19 symptoms.
However, amid the pandemic, it’s important to make modifications to sleep apnea treatment. Recommended guidelines for managing sleep apnea medical care during the pandemic include:
-
Restricting CPAP treatment to severe cases of sleep apnea
-
Viewing CPAP as an initial therapy for respiratory failure in certain COVID-19 cases
-
Promoting consistent use of CPAP devices
In the realm of advancing translational sciences, it’s about adaptability and resilience, traits that are crucial in the face of an unprecedented health crisis. The pediatric focused research network plays a significant role in this field.
Summary
As we navigate the intricate labyrinth of COVID-19 and sleep apnea, it becomes clear that understanding the interplay between these two conditions is critical. From shared risk factors and comorbidities to the impact of sleep apnea on COVID-19 severity, every piece of the puzzle adds to our understanding. While long COVID and sleep apnea can create a vicious cycle of persistent symptoms and mental health impacts, careful monitoring and appropriate treatment can lead the way towards better health outcomes. In the face of the COVID-19 pandemic, it’s not just about surviving, but thriving, and understanding the relationship between sleep apnea and COVID-19 is a step in the right direction.
Frequently Asked Questions
Is Covid causing sleep apnea?
Some COVID-19 survivors may experience sleep disturbances, including insomnia and new-onset nightmares. There is also a potential connection between COVID-19 and sleep apnea due to weight gain and prolonged illness.
How long will it take to reverse damage from sleep apnea?
Treating sleep apnea with CPAP for just 12 months can almost entirely reverse damage done to white matter, improving sleep and symptoms while decreasing cognitive risks.
What is the average age of death for sleep apnea?
The average age of death for sleep apnea is around 66.8 years, ranging from 42 to 86 years. This shows that sleep apnea can impact mortality across a range of ages.
How I cured my sleep apnea?
To cure mild obstructive sleep apnea at home, you can try natural remedies such as weight loss, making healthy lifestyle changes, sleeping on your side, elevating the head of your bed, playing a wind instrument or singing, and using oral or dental appliances. These methods can help improve your condition and alleviate symptoms.
Is sleep apnea a symptom of Long COVID?
Yes, sleep apnea can be a symptom of Long COVID, as indicated by a 35% prevalence of newly diagnosed obstructive sleep apnea in patients with lingering COVID-19 symptoms of fatigue or sleepiness.